Introduction
Essential thrombocythemia (ET) is a myeloproliferative neoplasm characterized by significant thrombocytosis with high propensity for thrombosis formation as well as other vascular complications. Most myeloproliferative neoplasms including ET are associated with Janus kinase ( JAK2) mutation. Other commonly associated mutations include Calreticulin ( CALR) and Myeloproliferative leukemia virus oncogene ( MPL) mutations. About 17% of cases of ET lack mutations in these driver genes. This presents a clinical conundrum for clinicians on initiation of appropriate treatment for these patients. We report a rare presentation of triple-negative ET with splenic infarction.
Case Summary
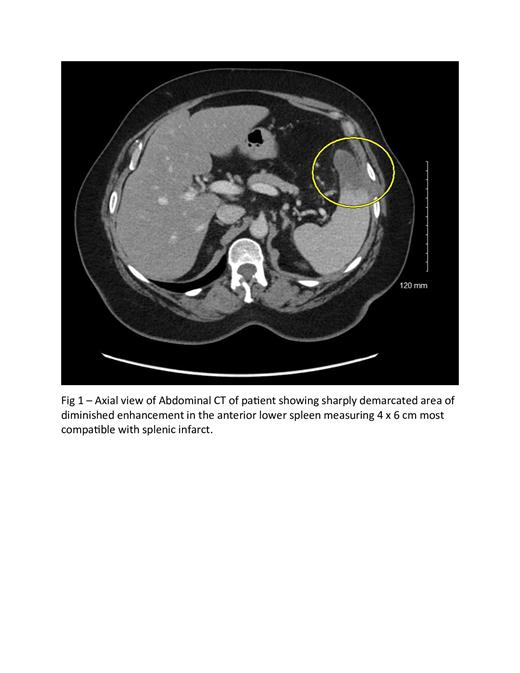
A 66-year-old Hispanic female who presented with left sided abdominal pain that gradually worsened over the course of 1 week; she believed it was stomach cramps. Laboratory evaluations were pertinent for platelet counts of 2000 x 10 9/L, hemoglobin level was 10.9 g/dl, and leukocytosis (white blood cell count 13.2k/uL) without left shift. Further work-up with iron studies was unremarkable and molecular studies were negative for BCR-ABL 1, PDGFR alpha/beta, FGFR 1, JAK2 V617F (including exons 12-13), CALR and MPL. A bone marrow biopsy showed an increase in megakaryocytes with some atypical forms with “enlarged size and nuclear hyper lobulation, and mild patchy reticulin fibrosis” suggestive of myeloproliferative neoplasm. Computed Tomography of the abdomen and pelvis with contrast showed evidence of splenic infarct. The patient was started on oral aspirin 81mg and oral hydroxyurea 2000 mg daily. Due to poor response to hydroxyurea and aspirin, she eventually had two cycles of platelet apheresis, and her platelet count improved to 1000 x 10 9/L. A repeat bone marrow biopsy was subsequently done to confirm essential thrombocythemia. At the time of discharge, the patient was asymptomatic and platelet count had decreased to 892 × 10 9/L.
Discussion
Essential thrombocythemia (ET) is a rare but recognized cause of vascular complications including arterial and venous thrombosis. Triple negative ET is quite uncommon and can pose a great deal of diagnostic challenge which can impact timing of initiation of appropriate therapy. This clinical vignette exemplified the conundrum encountered in making a diagnosis of triple negative ET. Following the World Health Organization (WHO) 2016 criteria for diagnosis of ET, patient has to have all 4 of: sustained platelet counts >450 x 10 9/L, bone marrow biopsy showing increased number of enlarged and mature megakaryocytes with no significant increase or left shift of granulopoiesis or erythropoiesis, presence of driver mutations/clonal markers (including JAK2, CALR and MPL mutations) or absent of evidence of iron deficiency or cause for reactive thrombocytosis and not meeting WHO criteria for Polycythemia vera or other myeloid neoplasms.
Our patient met criteria for ET with no driver mutation detected, hence triple negative ET. She was also classified as high-risk ET using the revised International Prognostic Score for Essential Thrombocytopenia (IPSET). Initial work up of this patient was not confirmatory of the essential thrombocythemia due to the bone marrow biopsy not clearly defining features as per WHO stipulations, thus, a more aggressive therapy was not pursued. This can pose a great deal of diagnostic challenge which can impact timing of initiation of appropriate therapy. This is not uncommon especially considering sampling challenge. Studies has shown that early initiation of cytoreductive therapy prophylactically in a high-risk patients can avert vascular complications of ET (including splenic infarction). The index patient responded slowly to platelet apheresis which can be an effective treatment in acute thrombotic complication of ET.
Conclusion
The diagnosis of triple negative essential thrombocythemia can pose a clinical challenge which impacts effective management of this myeloproliferative neoplasm. There is a dire need for further discussion on this conundrum to provide more applicable recommendations to avert the rare but fatal complications of ET. Platelet apheresis can be an option for emergency treatment in patients presenting with a major vascular complication like splenic infarction.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal